Quality Payment Program (QPP)
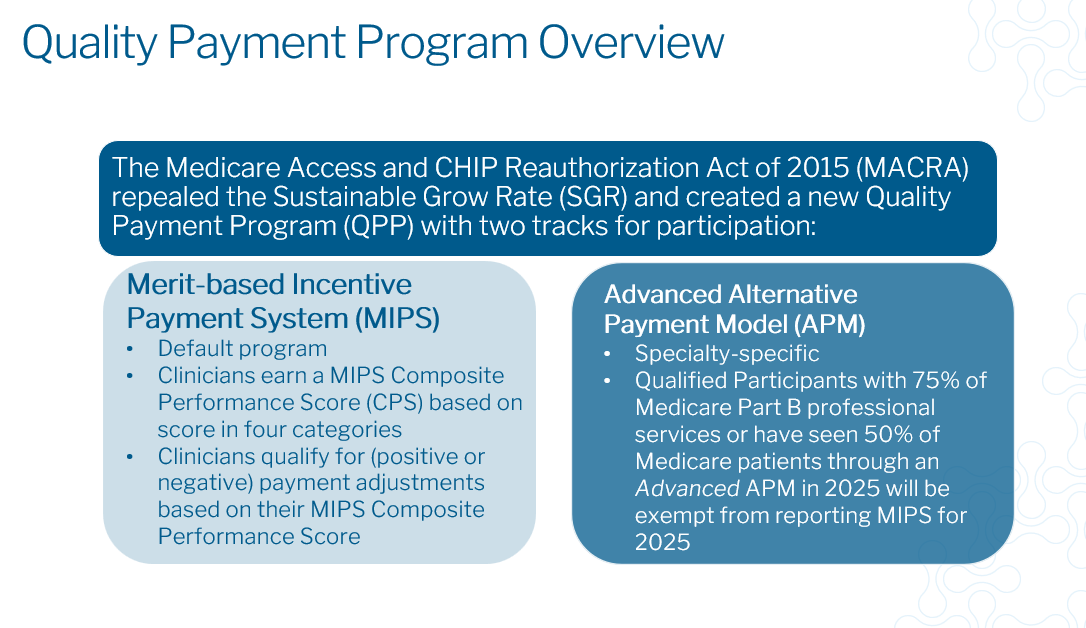
In 2017, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) established the Quality Payment Program (QPP) which replaced the Sustainable Growth Rate (SGR) as a basis for clinician payments.
CMS has state that their goals for the MACRA program are:
To improve beneficiary population health
To improve the care received by Medicare beneficiaries
To lower costs to the Medicare program through improvement of care and health
To advance the use of healthcare information between allied providers and patients
To educate, engage and empower patients as members of their care team
To maximize QPP participation with a flexible and transparent design, and easy to use program tools
To maximize QPP participation through education, outreach and support tailored to the needs of practices, especially those that are small, rural and in underserved areas
To expand Alternative Payment Model participation
To provide accurate, timely, and actionable performance data to clinicians, patients and other stakeholders
To continuously improve QPP, based on participant feedback and collaboration
There are two ways to participate in MACRA, the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs).
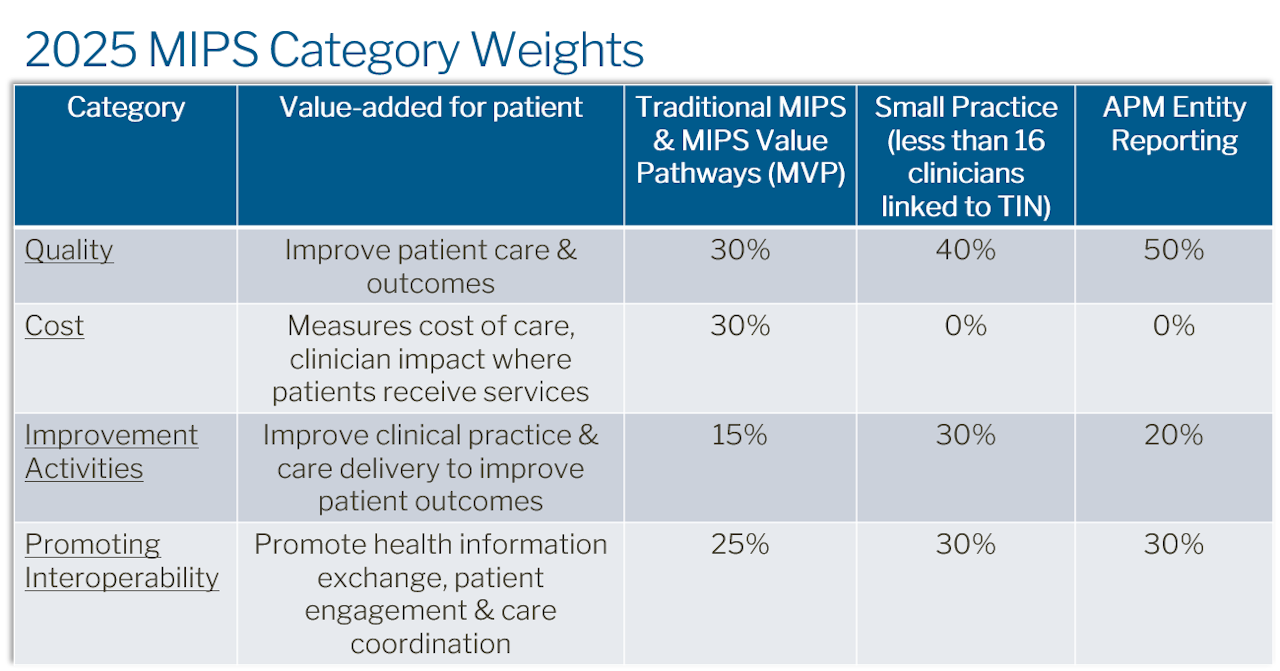
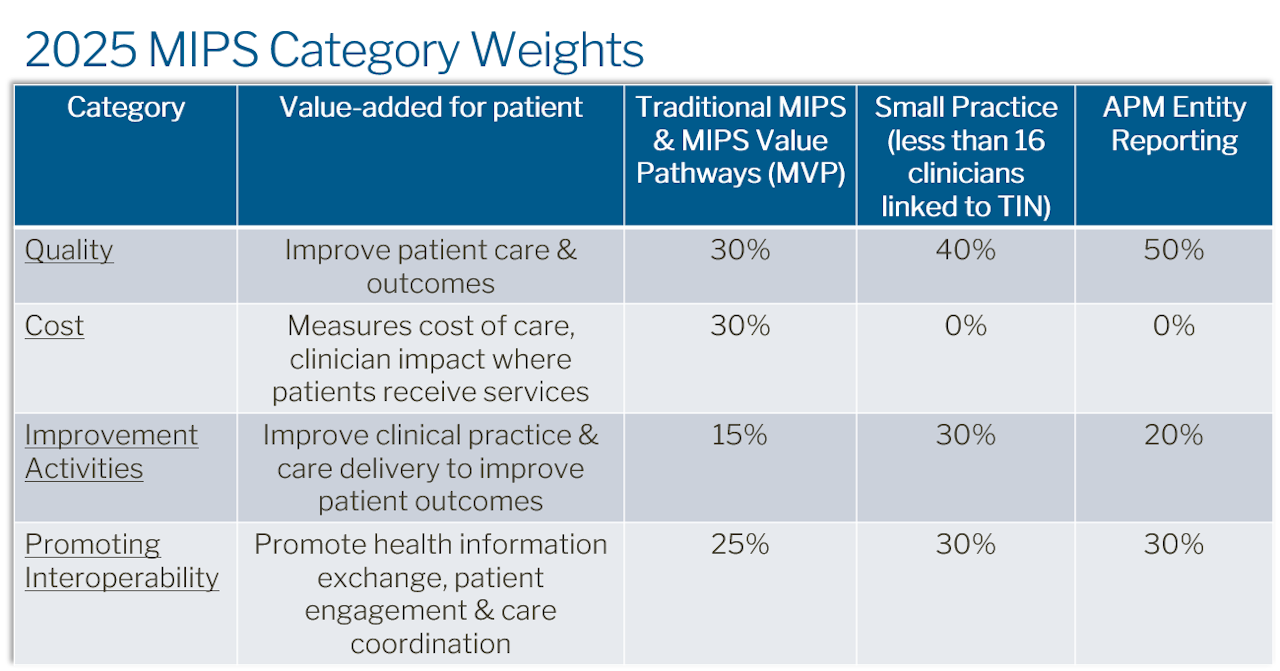
MIPS has 4 categories: Cost, Improvement Activities, Promoting Interoperability, and Quality.
Click on a category below to explore more details.